By Jeffery E. Stern

The tiny village of Meliandou, nestled in the Forest Region of southern Guinea, has begun to see flashes of the outside world. A Messi soccer jersey, three sizes too big, on a little boy. A down parka on an old man in the heavy heat, worn as a robe of distinction. You might even come across the occasional teenager on a cell phone, cupping the device from the sun as if lighting a cigarette in the wind. But mostly it is a place from the past–a rutted dirt path between thatch-roofed shacks, on a hillside sloping up toward the forest. It is home to just a few hundred people. Chickens and goats wander freely. Local shamans are the first responders when illness strikes.
In Meliandou, bushmeat has long been a common source of food. As elsewhere in West Africa, hunters wade into the forest and come back with whatever they can find. Once, not so long ago, what they found was a rich and varied bounty: monkeys, antelope, squirrels. That has changed; the whole eco-system has re-arranged itself. After civil wars broke out in Liberia and Sierra Leone, refugees poured over the borders, and the population grew, even as a power struggle in Guinea took an economic toll. People started looking to the rich resource all around them: trees. Trees were felled to make way for farms or burned down for charcoal. Endless truckloads of timber were shipped to construction companies. The forest suffered another trauma as mining interests–the Anglo-Australian Rio Tinto, the omnipresent Chinese–pushed aggressively to exploit the country’s natural resources (bauxite mostly). As the forests disappeared, so too did the buffer separating humans from animals–and from the pathogens that animals harbor.
Ordinary life in Meliandou came to an end on the day last December when the Ebola virus, which had last claimed a fatality thousands of miles away, arrived in the village, most likely in the body of a fruit bat–its natural non-human reservoir, according to a virtual consensus among scientists. Mining and clear-cutting had driven bats from their natural habitats and occasionally closer to people, like those of Meliandou. And fruit bats love palm and mango, which ripen in the village’s remaining trees. Bats also feed in colonies, which makes them tempting targets: a single shotgun blast can bring down 10.
Ebola is one of the deadliest viruses known to medical science, with no specific cure and mortality rates of up to 90 percent. The Ebola epidemic now raging in West Africa is the worst one in history. It has decimated Meliandou and moved far beyond. But the mystery today is not how the epidemic began–it is why a concerted effort by an army of international experts was unable to stop it. Part of the answer is the chameleon-like character the virus displays in this part of the world. An even larger part lies in the international response itself. It was rapid and comprehensive–exactly what you would hope. But there was an unexpected reaction that undermined everything the experts sought to achieve–and at the same time fooled many of them into thinking they had succeeded in their aims. Eventually they understood the truth. By then it was too late.
On the Move
As near as anyone can tell, the outbreak started when a few tiny rod-shaped particles–each merely an attack plan coded in ribonucleic acid and wrapped in a protein shell–found their way from a fruit bat into the body of a child not yet two years old. Perhaps, while the mother was preparing the day’s hunt, some of the bat’s blood was flung in the child’s direction. Perhaps, while the mother’s attention was elsewhere, the child touched the animal, then brought his hand to his mouth, the way babies do. Either way, a few strands of the Ebola virus attached themselves to cells in the child’s immune system and used the cells’ machinery to replicate. The boy developed a fever, then diarrhea and vomiting. His organs began to fail. He began to bleed internally and went into septic shock. In four days, he was dead.
It might have ended there–one child’s death in the jungle, way back in December–with no one ever to know that Ebola had spilled over into the human population. Certainly this happens often–spillovers that produce outbreaks so sudden, and generally so remote, that they don’t spread. People close by attribute the deaths to some other, more common affliction, while people far away never hear about them at all.
In this case, however, a family dispute intervened. After the child was infected but before he died, the mother, who happened to be pregnant, packed up the boy and a daughter and marched across the village to her own mother’s house. Space there was tight, because the grandmother had a houseguest. Beds were shared, and the baby’s symptoms exploded. His mother was infected, his sister, his grandmother, the houseguest too. When the mother miscarried, the midwife was infected. The Ebola virus had started to move.
When Ebola strikes, it kills quickly, but it can take up to three weeks to incubate, and usually around 10 days. The period is long enough that contact with a possible source may have been forgotten, and long enough for infected people to travel without symptoms. And even if you tested for Ebola–which nobody in Guinea had the capacity to do–you wouldn’t find it during the incubation period: Ebola can’t be detected in the blood until symptoms show. An epidemic can start slowly and go unnoticed for weeks. This has never been much of an issue before, because Ebola tends not to find its way into large population centers, or places where people are very mobile. This time would be different.
On January 24, more than a month after the first infection, Jean Claude Kpoghomou, a doctor in the town of Tekolo, called a superior to report on something strange happening in a village under his jurisdiction. Three patients had died in the span of two days, he said. All of them came from the same village, a place called Meliandou. The symptoms looked like cholera: diarrhea, vomiting, extreme dehydration. Cholera outbreaks were not uncommon in Guinea. An especially devastating outbreak had occurred just two years earlier, and Meliandou had even been one of the villages targeted for a public-health education campaign. A big pictographic billboard was installed at the entrance to the village, with explicit instructions for the mostly illiterate villagers about how to avoid contaminating the water supply. Dr. Kpoghomou’s superior forwarded the alert from Tekolo on to the health department’s prefectural authority in Guéckédou. Guéckédou sent the alert up to the regional director of health in Nzérékoré, who sent it on to the Ministry of Health in Conakry, the country’s capital, a city of a million and a half on the coast several hundred miles away. The national government had now been alerted: a potentially serious crisis was developing down in the Forest Region.
Mistaken Identity
A mid the constellation of public-health crises that Guinea must contend with–under-resourced and overburdened as it is by a constant onslaught of ordinary killers like malaria, tuberculosis, and automobiles–it was not surprising that three deaths in the Forest Region did not warrant immediate intervention. But officials in Guéckédou organized their own small investigative team and dispatched it to Meliandou.
Here, then, still in January, long before the outbreak took off, a team of doctors stood at ground zero, staring at some of the first casualties. They had no idea what they were looking at.
The way Ebola kills would seem impossible to mistake. What the casual observer knows of Ebola are its most spectacular cases, or the cinematic depictions of them: prodigious bleeding from eyes, ears, nose, anus, and nipples. Symptoms like these, presenting all at once, would be impossible to miss or misinterpret. But not every Ebola case ends with such a biblical scourge, and many of Ebola’s symptoms are identical to those brought on by other diseases. Until its final stages, Ebola can easily be mistaken for cholera. It can also look a lot like malaria, another long-tenured killer in Guinea. What no one has ever died of anywhere close to Guinea is Ebola. The last big Ebola outbreaks–in Uganda and the Democratic Republic of the Congo in 2012–were more than 2,000 miles away. They might as well have been in another world. If you’d told any of the investigators, as they considered the crisis developing in Meliandou, that they were looking at Ebola, they either would not have believed you or, just as likely, would have asked you what Ebola was.

On January 26, officials at the prefectural health authority held a meeting in Guéckédou. They now knew that something was wrong in Meliandou, but they didn’t know what. They consulted foreign health professionals stationed in town; Doctors Without Borders, or M.S.F. (for its French name, Médecins sans Frontières), had a malaria project there. Officials decided to make another visit to the village, this time with a more experienced medical team, on January 27.
For a second time, health workers stood at the epicenter of the Ebola outbreak, and for a second time they did not understand what they saw. By now there had been eight Ebola infections and seven deaths.
Meanwhile, the virus had slipped out of the village. When the grandmother of the infant victim fell sick, she decided that the way the villagers were approaching the illness–summoning a shaman to brandish his fetishes and work his spells–was not satisfactory. The grandmother had a friend in Guéckédou who was a nurse, and when the grandmother’s symptoms began to worsen, she went to see what real medicine could do for her. The nurse tried to help, but he had no idea what he was dealing with. The grandmother went back to Meliandou, where she died.
In early February, the nurse himself developed a fever. Now the virus was in Guéckédou, a bustling trading hub where people converge from Liberia and Sierra Leone. When the nurse’s condition deteriorated, he sought help from a friend who was a doctor in Macenta, in the next prefecture over. The nurse stayed just one night in Macenta–sleeping in the doctor’s own house, sharing a room with the doctor’s own son–and died the next day, February 10, in the waiting room of the local hospital’s lab. The doctor in Macenta was shocked. He didn’t know what he had just witnessed, but it was unlike anything he had seen before, and he immediately sent an alert to the regional director of health in Nzérékoré. Then the doctor developed a fever. He set off for the capital, where he hoped someone might have answers. But along the road–a jolting, treacherous passage lined by burned-out cars and always a few freshly rolled tractor-trailers spilling timber–the doctor died. His body was sent to Kissidougou, a city of more than 100,000, where a funeral was held. Before long, Kissidougou was experiencing an outbreak of whatever it was that had killed the doctor.
If the virus had failed in its first attempt to reach the capital, it was gaining momentum elsewhere, spreading through the forest and venturing dangerously close to international borders.
At the hospital in Guéckédou, more and more people were showing up with vomiting and diarrhea. Looking at the nine cases of reported cholera in his wards, a doctor named Alexis Traore began to feel that the diagnosis might be wrong. The staff was highly sensitized to cholera–appropriately so, given the outbreaks they had endured–and the patients had telltale symptoms. But one symptom didn’t fit: the patients all had fevers. Fever generally isn’t associated with cholera. And Dr. Traore saw something else inconsistent with cholera: one of the patients was bleeding from the nose.
Just as Traore began to challenge the diagnosis of cholera, his inquiry was foiled: tests the hospital had run for cholera came back, and seven of the nine were positive. The tests the hospital ran were cheap, easy to use, and highly sensitive; they are designed never to let a possible case elude detection. The downside: more than a few false positives. What this meant for Dr. Traore was that the working diagnosis had to remain unchanged: cholera. He notified his superiors in Nzérékoré.
Nzérékoré had just received a report from Macenta, which was reeling from its own tragedy. The doctor who had fallen ill and died on the way to Conakry–he was just the beginning. Mysteriously, the doctor’s son had also died, and a colleague of the doctor’s who worked in the hospital lab, along with two of the doctor’s brothers and a nurse he had treated. Something was killing people in Macenta. Nzérékoré compiled a report on the two separate crises and sent it up to the capital.
In Conakry, news of a doctor’s death was finally enough to register with the authorities. No one yet knew, but by now Ebola had claimed close to 30 lives and was continuing to spread–to Dandou Pombo, Dawa, Gbandou, Farako, and Baladou. The Ministry of Health and the country office of the World Health Organization set up a joint investigation, sending medical personnel to record the symptoms and backgrounds of patients who had died in Macenta. In the process, the team discovered that one of the victims–the nurse–didn’t live in Macenta but rather had come from Guéckédou.
This was a crucial fact: the team began to suspect that the separate crises in Macenta and Guéckédou were not separate at all. Whatever was happening in the Forest Region, it was a single phenomenon. The team wrote up its findings and sent them back to the capital, where a few doctors began to suspect that the culprit wasn’t cholera or malaria–some even venturing that the disease might be a hemorrhagic fever.
Here, nature threw one more curveball. Guinea, Sierra Leone, and Liberia have the world’s highest incidence of Lassa fever, a less lethal virus that can also produce hemorrhaging. So when a hemorrhagic fever was suspected, that is where the finger of evidence logically seemed to point–toward Lassa.
Three and a half months into the outbreak, no one suspected Ebola.
Collecting Samples
What finally gave the virus away was, of all things, hiccups. On March 14, M.S.F.’s Geneva office received a report from a medical investigation in Guinea. M.S.F. Geneva immediately forwarded the report to Dr. Michel Van Herp, an epidemiologist in its Brussels office, and one of the world’s leading experts on Ebola. When Van Herp opened the document, what immediately jumped out at him was that half the victims had developed hiccups. For reasons not entirely clear to the medical community, hiccups are associated with Ebola. “It is definitely a hemorrhagic fever,” Van Herp told a colleague in Geneva, who was consulting with him by phone. “But we must really take into consideration that it is worse than Lassa. I think it’s Ebola.” Van Herp notified M.S.F.’s Brussels headquarters, presented his suspicions, and then immediately began preparing to leave for Africa.
That same evening, working on the doctor’s hunch, M.S.F. initiated its response. A team on the ground in Sierra Leone was redirected across the border to Guinea with some basic equipment and protective gear. The team was prepared to deal with Lassa, so was not equipped for a sustained response to Ebola, but had enough to make do for the moment. A separate team was assembled in Brussels and made ready to travel. M.S.F. also needed to get blood samples to a lab capable of testing for Ebola and other exotic pathogens. To that end, a charter plane was dispatched from Conakry to an airstrip outside Guéckédou. Blood samples with suspected Ebola virus are categorized for transport by a special code, UN 2814, indicating “infectious substances, affecting humans,” and M.S.F. hired a specialty logistics operator to send the samples, which were packed according to a strict protocol, with three layers of protective and absorbent material. Then–because it was simply the fastest way–the samples from Guéckédou were loaded onto the daily Air France red-eye from Conakry to Paris.
Nobody knew that, as the Air France flight left Conakry, the first infected person had already arrived in the capital–a trader with ties to the Forest Region. In a little more than a week, the virus carried by the trader would infect five other people. Within a month, the number would reach 47.
In Paris, the samples were taken to the Institut Pasteur. But the institute reported a technical problem at the lab and had to move the samples to another facility, 250 miles away, in Lyon, where technicians were put on alert and told to wait up. Once the samples arrived, the technicians worked into the night. By a little after two A.M. on March 20, they had the first results: what they were looking at was a filovirus, meaning it couldn’t be Lassa. Later that day, at seven P.M., the worst was confirmed: the samples were positive for Ebola. The lab notified M.S.F., which notified its team on the ground and the government of Guinea. On March 22, more bad news came from the lab. The samples from Guinea were the Zaire strain, the deadliest known version of the virus.
Connecting the Dots
When the international community responded to the Ebola outbreak, it did so with astonishing speed. One reason for this was the effective coordination by groups such as M.S.F. But there was another reason behind the rapid response: the sheer horror of Ebola has given it a certain cachet. Epidemiologists who study and follow the virus–people such as Michel Van Herp, of M.S.F., and Pierre Rollin, of the Centers for Disease Control and Prevention–constitute something of an exclusive group whose members stand ready to fly anywhere at a moment’s notice whenever Ebola turns up. Because Ebola outbreaks can kill so quickly, there’s an urgency to get on the ground and begin the work of containment immediately. And because they are also rare and usually very remote, they evoke an eagerness, not unlike that of astronomy enthusiasts rushing to witness some rare astral event.
From a scientific point of view, the Ebola virus is intriguing: a contradiction lies at its core. On the one hand, there is something intentional about a virus that creates in its host precisely the conditions it needs to travel. Ebola can pass from one host to another only through direct contact with an infected patient’s bodily fluids, and once it is inside a human body, it activates several different mechanisms that cause a host to release bodily fluids in several varieties. On the other hand, it’s not contagious enough, typically, to compensate for the speed with which it kills. It can’t move through the air; it can’t live in the water. It can be transmitted only when the host is symptomatic, at which point the host will likely die so quickly that the virus doesn’t have much of a chance to lodge someplace new. But its chances of survival improve markedly if it strikes in a part of the world–like Guinea–where funerals tend to be intimate affairs; where the family lays its hands on the deceased, and sweat, tears, and other fluids have the chance to mix. Then, killing the host becomes not a dead end for the virus but an opportunity to travel further.
As M.S.F. continued to mobilize– it would have 60 staff members on the ground in little more than a week–others were making arrangements as well. Under the auspices of the Emerging and Dangerous Pathogens Laboratory Network, an all-star team of lab technicians from all over Europe was assembled in Munich and then dispatched to Africa carrying an entire lab piecemeal as their checked luggage. The Centers for Disease Control and Prevention rushed to complete a computer program it had been developing to track outbreaks; the program needed to be translated into French so it could be used in Guinea. The C.D.C. also dispatched a team, which grew to more than a dozen and was led by Rollin, who arrived in Guinea on March 30. Some 3,000 biohazard suits were flown in. Experts and volunteers poured in from the World Health Organization and the Red Cross.
With help from the W.H.O. and M.S.F., the Ministry of Health set up the “115” Ebola hotline; when a call came in, the ministry would dispatch a doctor on a motorcycle. If the doctor believed a case could indeed be Ebola, he called back to his dispatcher, who then called M.S.F., which in turn sent a team to the scene in full biohazard gear to collect the patient. At the same time, information about Ebola blanketed the country: to get cooperation, you need to explain the gravity of the situation. People all across Guinea were soon told that the virus was highly contagious, that the mortality rate was 90 percent, and that there was no cure–exaggerated versions of the truth, but a message that sank in. Meanwhile, the international groups began the detective work of uncovering the transmission chain, tracing every case back to the origin, an exhausting, tedious game of connect the dots, but a critically important one. If there’s a dot you cannot connect–a patient with no apparent link to any other patient–it doesn’t mean there isn’t a link. It just means you haven’t found it yet. An unconnected dot may mean that an entire branch of the outbreak is out of sight.
Ministry of Fear
By mid-April, Dr. Abdourahammane Batchyli, then working for the Guinean Ministry of Health’s national Ebola-oversight division, was spending his days in his Conakry office fielding calls from the 115 hotline and listening to excited citizens offering fantastical explanations for what was happening around them. A member of the Fula ethnic group, a rival of the sitting president’s Malinke group, explained to Batchyli that “this outbreak isn’t real–how could we be having Ebola here? President Condé made it up because he’s trying to delay elections.” Another said the president had introduced the virus to exterminate the Kissi tribe. A man claiming to be a spiritual guide called to say the epidemic was a plague visited upon the people of Guinea when a certain white snake was killed; it could all be cured by sacrificing seven cows.
At first the theories didn’t bother Batchyli very much. There were those who didn’t believe the outbreak was real. But most did, and took it seriously, which was the important thing; their musings about its origins were secondary. It didn’t matter if people weren’t thinking rationally. Who was? It wasn’t just illiterate villagers who acted out of fear. Educated people were scared. He was scared. So were foreigners: On April 1, Saudi Arabia had stopped issuing hajj and umrah visas to Guineans and Liberians, which meant that people in predominantly Muslim Guinea could not go on the pilgrimage to Mecca. On April 4, passengers on the Air France flight from Conakry were quarantined when the plane landed at Charles de Gaulle Airport, in Paris, and not allowed to leave until each was checked for fever, all because someone had gotten sick in the lavatory. Emirates airline had stopped flying to Guinea. Mining companies had pulled out their foreign staff. In the capital, radio stations were broadcasting ads for the best brands of chlorine, to protect yourself from Ebola, and Batchyli saw an article about “rebels dressed in yellow who attacked Guinea and then disappeared”–the interpretation of a local journalist trying to make sense of all the people in big yellow protective suits who had suddenly descended on the country.
But what soon became troubling to Batchyli were the phone calls from people who saw the hand of foreigners behind the epidemic. The logic followed a pattern: the virus had never been anywhere near Guinea before. Then the white people came, and only at that point did talk of “Ebola” start. The foreigners had come so fast that they had actually out-run their own messaging: there were trucks full of foreigners in yellow space suits motoring into villages to take people into isolation before people understood why isolation was necessary.
Even if you understood the reasons, the message from the government and the health workers (and the local media) had undercut the incentive to cooperate. If Ebola was a death sentence, what was the point? The public-service announcements had not been subtle–they didn’t explain that mortality rates vary or that, with supportive care, patients do survive (as half the Ebola patients at the M.S.F. treatment center in Conakry had done). To a villager, the isolation centers were fearsome places. They offered a one-way maze through white tarpaulins and waist-high orange fencing. Relatives or friends went in and then you lost them. You couldn’t see what was happening inside the tents–you just saw the figures in goggles and full-body protective gear. The health workers move carefully in order to avoid tears and punctures; from a distance, the effect is robotic. The health workers don’t look like any people you’ve ever seen. They perform stiffly and slowly, and then they disappear into the tent where your mother or brother may be, and everything that happens inside is left to your imagination. Villagers began to whisper to one another–They’re harvesting our organs; they’re taking our limbs.
The process of finding and isolating infected patients was on one level effective and on another deeply disorienting. Batchyli didn’t fully grasp the implications at the time. Nobody did. But people in Guinea were as frightened by the response to Ebola as they were by Ebola itself. As the international community started to make significant progress against the epidemic, people in the Forest Region and in the capital were starting to shut health workers out. Fear was proving to be a contagion: You want to hide from the disease. You want to deny that you have it. You want to retreat to your village behind a phalanx of family members, and when the men in space suits come looking for you, you want to crawl under the bed. And you do–and your family members throw stones at the people in space suits, and so they leave.
This dynamic did not at first register. What the medical teams in Guinea saw was that, barely a month after the international community’s response began, the incidence of reported infections stopped rising, then declined. It continued to drop. In early May, the Ebola-treatment center inside Donka hospital, in Conakry, reached a milestone: a full week had elapsed since its last Ebola case. Another week passed, with nobody testing positive. The work until then had been so intense and so extraordinarily draining–working in the heat in full Tyvek suits, treating patients who often died and who posed a direct threat to care-givers–that the mood after two Ebola-free weeks was one of relief, bordering on celebration.
Another week passed in Conakry with no Ebola victims. Things slowed even further. A few patients came in and were triaged to the “suspected” section of the treatment center; none tested positive. Relief gave way to boredom. The medical team began making work for itself–taking a full inventory of supplies, cleaning and re-disinfecting tents.
Yet another week passed: once again, Ebola-free. Then, in late May, more good news. At the daily coordination meeting, a Ministry of Health representative announced that the last outstanding contact had been symptom-free for 21 days. The implication was clear: if everyone who had come into physical contact with an Ebola patient was symptom-free after the virus’s incubation period had expired, there effectively was no one left who could be infected.
In Guéckédou, medical personnel received the news from the capital by phone. There were still a few patients at the treatment center there, but after an onslaught of 163 Ebola cases in that one prefecture, 119 of them fatal, the team was now following contact cases in only two villages. The news from Conakry tracked with what they were seeing in the Forest Region.
The President of Guinea announced that “for the moment, the situation is well in hand.” The foreigners began to leave. The C.D.C. cycled its staff out of Guinea. At the treatment center at Donka hospital, preparations went forward to hand leadership over to local staff. By this point, toward the end of May, there had been 248 clinical cases of Ebola throughout Guinea, and 171 deaths. But there were no more cases in the pipeline. The worst was over.
Much of the medical community in Conakry savored a moment of respite. But it was illusory. As the doctors would learn all too soon, many people had simply stopped cooperating with health workers. They had gone to ground and taken Ebola with them–until so many people had become sick in a community that it was no longer possible to conceal them.
On May 27, a patient with Ebola was admitted to the treatment center in Conakry–the first such patient in a month. On June 2, five more people with Ebola were admitted. On June 3, two more arrived. The cases weren’t coming from just Conakry. They were also coming from places a hundred miles or more from the capital: Télimélé, Boffa–everywhere. Down in the Forest Region, between May 29 and June 1, there were 15 new Ebola cases. Out of nowhere, from a flat bottom, the curve had begun to rise, and to rise more steeply than ever.
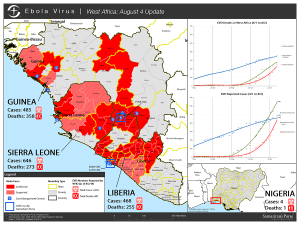
Until 2014, the deadliest Ebola outbreak on record had killed 280 people. As of this writing, 1,427 people have died from Ebola during the current West African outbreak, out of 2,615 confirmed cases. The outbreak has spread from Guinea to Sierra Leone, Liberia, and Nigeria. In early August, the World Health Organization convened an emergency meeting and declared a “public health emergency of international concern.”
In Meliandou, where the epidemic began, village elders say they’ve lost 40 people to the disease. Hunters have stopped hunting. The village has been isolated and ostracized. Moto-taxis are afraid to enter and neighboring villages refuse to trade. These days, the people of Meliandou are worried less about Ebola. Now they worry more about hunger.
The AfricaPaper – We are grateful to Jeffery E. Stern and Vanity Fair for this story focusing on Ebola in West Africa.